The Hidden Costs of Rapid Weight Loss While on GLP-1 Medications
Written by Christy Walowit, MS, RDN
GLP-1 medications like Ozempic, Wegovy, Mounjaro, and Zepbound were originally developed for treatment of type 2 diabetes, and have gained attention in recent years for their role in weight loss (Read more about GLP-1 Medications here). These medications are frequently prescribed to people in larger bodies, even if no health issues are present. This trend raises important questions about how we define health, and the potential benefits and risks of using GLP-1 medications. In this blog, we’ll explore GLP-1 use among folks without diabetes, risks of rapid weight loss, and implications for long-term health.
A quick note: Rapid, dramatic weight loss is not realistic for most individuals prescribed GLP-1 medications at clinically appropriate, evidence-based doses. Unfortunately, media stories and social media influencers can create unrealistic expectations that don’t reflect typical results. It's important to approach GLP-1 use with realistic expectations and work with your healthcare team to identify personalized treatment goals.
Energy Deficit and Metabolic Adaptation
A calorie restriction (or energy deficit) is a common weight loss strategy recommended by the dieting industry. An energy deficit may also occur as a result of using GLP-1 medications, due to hunger and appetite-suppressing effects. In the long-term however, losing weight due to not eating enough comes with risks, and can lead to weight regain. This is because of “metabolic adaptation,” an important and complex survival mechanism our bodies use to protect our health and wellbeing.
Here’s how it works:
When our bodies don’t get enough fuel, they interpret this as being subjected to a famine. Historically, famines have been a big threat to human survival, and our bodies have learned a few tricks to protect us from this perceived food shortage and ensure our safety. These powerful biological mechanisms include:
Slowed Metabolism: Our bodies may adapt to switch into an “energy saving” mode to store energy and encourage weight gain – back to your original weight, and often higher. Your body isn’t fighting you. It’s doing exactly what it was designed to do: protect you and keep you alive and thriving, even when fuel gets low.
Cannibalizing Muscle: The body will break down muscle to be used as fuel. Muscle is metabolically active tissue (meaning it helps us burn energy) and supports us maintain healthy blood sugar levels, protects our bones, and helps us participate in activities. It takes a long time to re-gain this muscle after the “famine” (or calorie deficit) ends. In general, exercising during a calorie deficit does not protect against this muscle loss or promote muscle gain – read to the end to learn more!
Fat Overshooting: When our bodies lose fat and muscle mass, it triggers our bodies to store more weight in the form of fat, rather than muscle. Fat is a form of storage energy – so of course our bodies would prioritize saving resources in times of scarcity!
Hormone Changes: When we are experiencing a calorie deficit, our bodies will send us hormone signals to increase food cravings and hunger signals. Symptoms of this may include frequent food thoughts (may feel obsessive), strong food cravings, high hunger, feeling out of control around eating. Drugs like GLP-1s may play a role in limiting these cravings and hunger signals, which could make it challenging to recognize when our body’s needs aren’t being met.
Calorie Restriction Causes Food Preoccupation
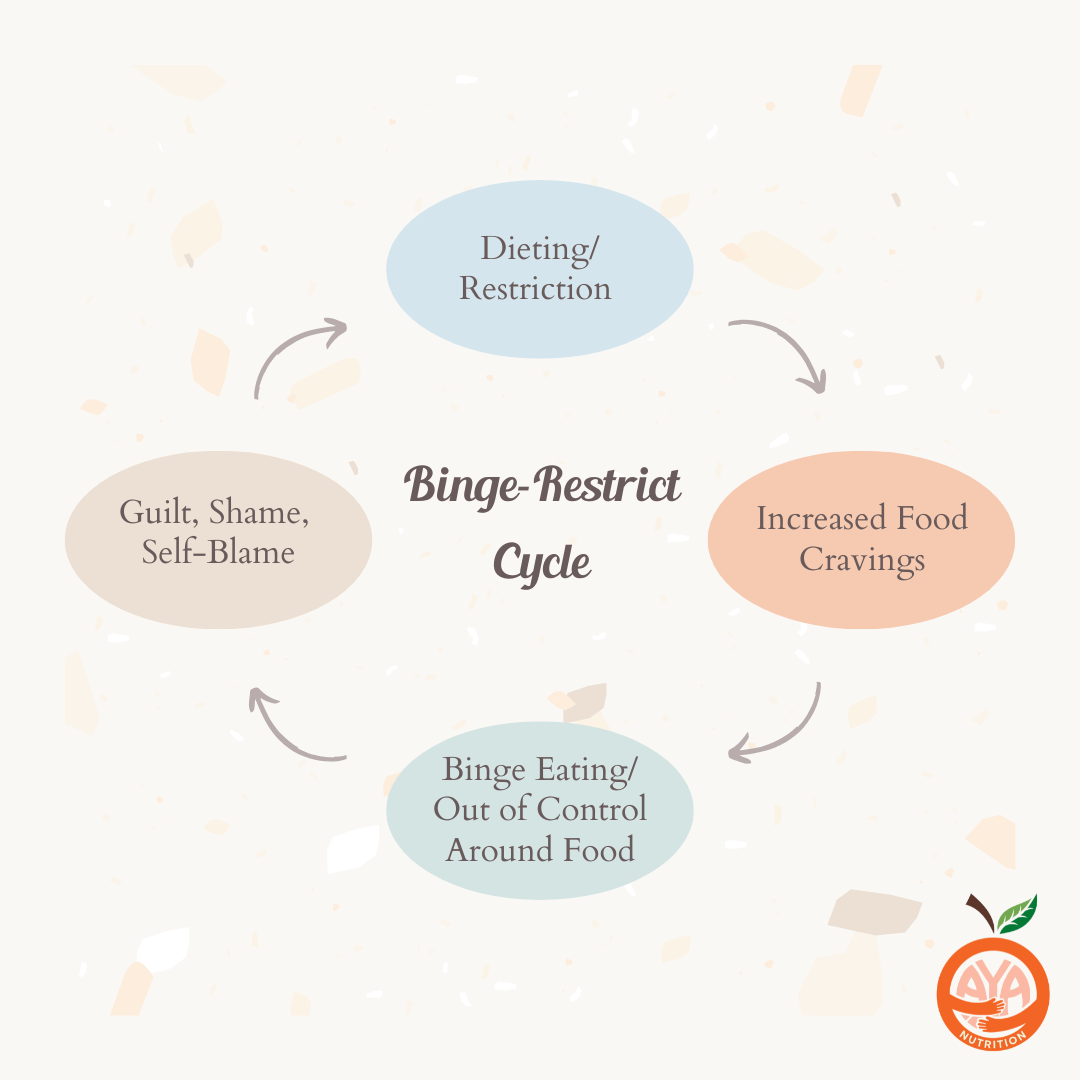
Regardless of whether there is an actual scarcity of food or a psychological sense of scarcity, a sense of food deprivation makes people feel obsessed with food. This is very common among those who have pursued calorie-deficit diets, experienced food insecurity, or have a history of an eating disorder. Calorie restriction can contribute to disordered eating, as it may lead to a restriction-binge-shame cycle that disrupts one’s relationship with food.
While GLP-1 medications may be effective in reducing the frequency or intensity of food thoughts, it does not address the underlying root cause and may be a temporary solution. Because not eating enough can cause frequent “food thoughts” or “food noise,” healing from this typically involves addressing the root cause and allowing yourself to eat and making peace with food (not more restriction!). Fortunately, this is highly treatable through collaboration with an intuitive eating-informed dietitian or therapist.
At As You Are Nutrition, we respect your decision to start–or not start–a GLP-1 medication, and our Registered Dietitians are trained to help you explore the underlying root cause of why these symptoms and food thoughts might be present to begin with. Read more about the signs and symptoms of dieting and calorie restriction here. This work does not need to be done alone!
Risks of Yo-Yo Dieting
Weight cycling, also known as “yo-yo dieting,” is the repeated cycle of dieting, weight loss, and regain. This often occurs as a response to weight loss or calorie deficit, when our metabolism slows down (think: “energy-storage-mode”) to compensate for not eating enough calories.
When weight loss is prioritized over health, the harms of weight cycling are often overlooked. Weight cycling comes with negative side effects such as shorter lifespan, increased risk of diabetes, high blood pressure, high cholesterol, and heart disease. It’s important that GLP-1 medications are not used as yet another yo-yo diet. It may be healthier to prioritize weight maintenance (staying at the same weight), than to gain and lose the same 10, 20, or 30 pounds again and again.
Gallbladder & Gallstones:
Our gallbladder has the important job of holding bile, a digestive fluid created by the liver that helps us to break down fats. Losing weight too quickly, or going long periods of time without eating can increase your risk of developing gallstones. This is due to the liver releasing extra cholesterol into the bile, or from the gallbladder being unable to empty properly. Weight cycling may also increase the risk of developing gallstones.
Malnutrition & Malabsorption:
GI symptoms, low appetite, and malabsorption associated with GLP-1 use can increase risk of malnutrition. Malnutrition is a serious condition that impacts every system in the body. GLP-1 medications can impact your body’s ability to absorb and utilize important nutrients such as protein, iron, vitamin B12, folic acid, vitamin D, and calcium. Rapid weight loss and GLP-1 use can increase the risk of malnutrition. At As You Are Nutrition, we recommend working closely with a Registered Dietitian to review blood labs prior to starting a GLP-1 medication, and completing periodic follow-ups to quickly identify and correct any nutrient deficiencies.
Exercise and Muscle Loss in a Calorie Deficit:
Overall, if we are not eating enough calories (aka: fuel!) and are losing weight, our body is breaking down fat and muscle to fill the “gap” in energy that we’re not getting from our diet. It makes sense that our bodies can’t use the food we’re eating to build muscle if it is in an active state of breakdown. In addition to fat and muscle loss, exercising in a caloric deficit can contribute to decreases in bone density and disruption of important hormones (such as IGF-1, which supports muscle growth and other important functions).
This is one of many reasons why weight loss doesn’t necessarily equal improved health, and we can’t choose what type of weight we are going to lose. For every 10 pounds of weight lost, approximately 3 pounds will be muscle loss - it’s a package deal!
Why is Muscle Important?
Muscle plays many important roles in our health, wellbeing, and quality of life. Muscle helps us build strong bones, improve strength, mobility, and overall health. It also helps increase our metabolism because it is considered “metabolically active” tissue. This means it helps our bodies use calories and keep our blood sugar in an ideal or target range. Not only does muscle support our blood sugar and other vital functions, but it can also help protect against “sarcopenia,” or age-related muscle loss. Sarcopenia can increase risk of falls, fractures, complications from surgeries, and mortality as our bodies age.
Fortunately, exercise and strength training are effective tools to increase muscle mass and may improve health when combined with adequate nutrition. We recommend working with a Registered Dietitian to help support your exercise goals and fueling needs.
Final Thoughts
Health is so much more complex than a number on the scale! Weight loss doesn’t necessarily equal improved health, and losing weight quickly can increase risk of disordered eating, gallstones, malnutrition, muscle loss, and other serious issues. Due to metabolic adaptation and our body’s powerful survival tactics, an energy deficit (from calorie restriction, GLP-1 medication, or other reasons) can actually promote additional weight gain in the long term. Although long-term research surrounding GLP-1 use among folks without diabetes is currently lacking, early research indicates weight regain may occur around the two year mark after starting a GLP-1.
GLP-1 medications may contribute to weight loss by reducing appetite and causing uncomfortable gastrointestinal symptoms, which can make it challenging to eat enough. If you choose to use a GLP-1, it’s important to nourish your body with enough food to help support your energy, strength, and overall well-being. Honoring your body’s nourishment needs can lead to more sustainable long-term health benefits than repeated cycles of restriction and regain.
Disclaimer: This content is for informational purposes only and is not intended to replace medical advice, diagnosis, or treatment. If you are struggling with an eating disorder or related health concerns, please consult a qualified healthcare professional, such as a doctor, therapist, or registered dietitian, for personalized guidance and support. If you need immediate help, reach out to a medical provider or a crisis support resource in your area.
References: